
Evaluation and Treatment Programs
The National Center for Women’s Health not only offers general obstetrics, gynecology and gynecologic surgery, but also specializes in the provision of care for patients with the following conditions:
- Infertility evaluation and treatment
- Prematurity Prevention Program
- Premenstrual syndrome
- Abnormal uterine bleeding
- Recurrent ovarian cysts
- Repeated miscarriages
- Dysmenorrhea and pelvic pain
- Surgical treatment of endometriosis
- Postpartum depression
- Progesterone support in pregnancy
- Perimenopausal/menopausal care
- Polycystic ovarian disease
- Reversal of tubal ligation
- Getting help
INFERTILITY PROGRAM
The Saint Paul VI Institute Infertility Program, one of the few that exists in the United States, is a disease-based approach which recognizes that “all infertility (or other reproductive problems) are caused by some type of organic or functional disease process.” Unlike the current medical approach which typically involves limited evaluation, patients at the Saint Paul VI Institute will receive a complete evaluation and a sound explanation as to why they are having problems achieving or maintaining a pregnancy. The organic or functional causes of infertility can be relatively easily diagnosed and treated.
Causes of Infertility (Organic or Functional)
- Endometriosis
- Pelvic adhesions
- Polycystic ovarian disease
- Obstructions of the fallopian tubes
- Hormonal dysfunctions
- Ovulation-related problems
- Previous chlamydia infections
- Hypothalamic amenorrhea
Infertility and related problems (such as repetitive miscarriage and tubal pregnancy) are best treated with a comprehensive approach to diagnosis and treatment. A typical evaluation includes serial hormone evaluation, a follicular ultrasound series, laparoscopy, hysteroscopy, and selective hysterosalpingogram. A seminal fluid analysis is recommended for the man if this has not been done. After evaluation, the physician conducts a comprehensive planning session with the couple during which the couple is shown the videotape of their laparoscopy and the various causes of the reproductive problem and the treatment plan for those difficulties are explained. Because it is a disease-based approach, the disease that caused the reproductive problem for the woman (and/or her husband) can be either eliminated or satisfactorily treated.
Effectiveness
By identifying and treating the underlying diseases that cause infertility, the Institute harnesses the
body’s ability to work more effectively as opposed to “driving” the reproductive system,
“pushing” the system, or trying to “replace” the system. The effectiveness of
the program varies depending upon the type of disease that occurs. In some cases, the Institute’s
effectiveness is greater than 80 percent in assisting a couple to successfully achieve a pregnancy. In
many common infertility problems, the success rate will be 50 to 75 percent. In some more
uncommon infertility problems, the success rate will be lower than that but almost always higher
than the rates expected from programs driven by the artificial reproductive technologies (in vitro
fertilization, artificial insemination, etc.). While the infertility program of the Saint Paul VI Institute
is one of the most successful in the United States, a pregnancy can never be guaranteed.
NaProTechnology-Driven
The new medical science of NaProTechnology is geared toward the evaluation, study and treatment
of reproductive and gynecologic problems. It allows for evaluation and treatment that are
cooperative with the reproductive system (which in this case is working abnormally). Thus,
pregnancy can occur with a normal act of sexual intercourse. The system is natural and is acceptable
to everyone. The treatments carry a very low incidence of multiple births and a low incidence of
subsequent tubal pregnancy and miscarriage–both are common problems associated with the
programs of the artificial reproductive technologies.
NaProTRACKING™ the Menstrual Cycle
Most infertility treatment programs in the country are based on artificial reproductive technologies
(such as in vitro fertilization, artificial insemination, selective abortion, etc.). In contrast, the
NaProTechnology-driven system of the National Center for Women’s Health is morally acceptable
to all people. For example, in vitro fertilization is a highly abortive technology that often forces
women to make abortion-related decisions, which they do not want to do. When quadruplets or
quintuplets result because multiple embryos were injected into the uterus, the proposed solution
is “selective reduction,” which is nothing more than an abortion. These are decisions
that most people do not wish to make and seem inconsistent for a treatment program that is
trying to generate new life while destroying new life. Because a NaProTechnology approach treats
the underlying diseases either medically or surgically, all pregnancies occur as the result of a normal
act of intercourse. The basic integrity of the unity which occurs with the natural achievement of
pregnancy is not compromised with the program found at the Saint Paul VI Institute.
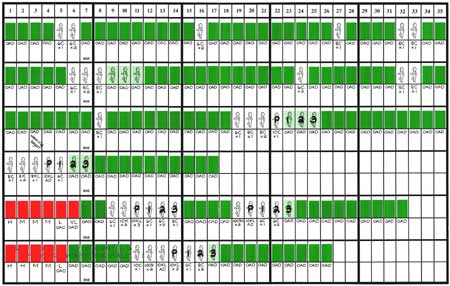
Because the woman is charting her cycles, very accurate hormonal evaluations can be accomplished and the various biological markers and their role in the infertility problem can be assessed. It is the most effective means currently available (including comparisons to urine test kits for ovulation) for determining the point in the menstrual cycle when a woman is fertile.
To learn how to NaProTRACK™ your cycles, enter Creighton Model FertilityCare™ System.
Affordable
Infertility treatment is often not covered by insurance programs. Artificial reproductive technology
programs run more than $10,000 per menstrual cycle and up to $150,000-$200,000 (or more) per
successful pregnancy.
At the Saint Paul VI Institute, evaluation likely includes NaProTRACKING™ the menstrual
cycle, a hormone profile, a follicular ultrasound evaluation, a selective hysterosalpingogram, and a
diagnostic laparoscopy. Test results might indicate the need for more treatment, including surgical
intervention. However, the overall cost of the program at the Saint Paul VI Institute is only a fraction
of the cost of a program that revolves around the artificial reproductive technologies.
Many couples come to Omaha for a 7-10 day stay to accomplish a complete infertility evaluation. The nurses will help you through this process and are available for any questions.
PREMATURITY PREVENTION PROGRAM
Prematurity, one of the major complications of pregnancy, affects approximately 10 percent of all pregnancies. Premature birth carries a significant risk of complications. In most circumstances, the best incubator for the baby is the mother’s womb. Modern medicine has not been able to duplicate the womb’s ability to care for the baby’s growth and development needs.
Premature birth also necessitates prolonged hospital stays for the baby, thus affecting the baby’s early infancy environment. While neonatal intensive care units are capable and the baby’s survival is good (especially after the 28th week), having a baby in intensive care decreases the ability of the parents to bond with the newborn and their ability to provide the newborn with the needed love and affection. Moreover, intensive care nursery is expensive.
For these reasons, a pregnancy should be maintained as long as possible (so long as everything else is normal). The Saint Paul VI Institute has introduced a Prematurity Prevention Program based on 20 years of research. While the national preterm birth rate is approximately 10 percent, the prematurity birth rate at the Pope Paul VI Institute is less than 4 percent. This is the result of an aggressive and pro-active management program.
Identifying Risk Factors
The most important factor in treating prematurity is identification of conditions associated with increased risk for premature birth. The Prematurity Prevention Program cannot eliminate the risk but does lower the risk of premature labor and subsequent birth. Risk factors include:
- Previous prematurity
- Exposure to Diethylstilbestrol (DES)
- Cervical incompetence (congenital, acquired, or family history)
- Previous repetitive miscarriages
- Placenta previa
- Malformations of the uterus or large uterine fibroids
- Cervical cone biopsy
- Multiple pregnancy (twins, triplets, etc.)
- Persistent uterine irritability
- Excessive amniotic fluid (polyhydramnios)
- Severe kidney or urinary tract infections
- Age less than 18 years or greater than 35 years
- Smoker
- Infertility or other reproductive disorders
- Low grade uterine infection
Self-Monitoring Your Uterine Contractions
Self-monitoring of uterine contractions is important in prematurity prevention. The Pope Paul VI Institute has developed a uterine contraction self-monitoring protocol, which is critical to pregnancy health maintenance. The woman self-evaluates her contractions, cramping, backaches, pelvic pressure, intestinal cramping, vaginal discharges, and vaginal bleeding. She looks for a change that occurs from day to day in the baseline of the general symptom pattern. This information is then shared with the physician.
Ultrasound Monitoring
Ultrasounds are performed at 6 to 8 weeks, 14 weeks, and 18 to 22 weeks to evaluate patients at high risk of preterm birth. Changes in the cervix, which have been undetected by the obstetrician till now, can be detected many weeks prior to the onset of preterm labor. Detection of dramatic changes allows for implementation of treatment options.
Treatment Approaches for the Prevention of Preterm Birth
For patients that exhibit increased uterine contractions during the course of their pregnancy and exhibit those signs that are suggestive of an increased risk for preterm labor, the physician will implement a number of treatment options. These treatment options may include the following:
- Bed rest
- Hydration
- Urinalysis
- Progesterone therapy
- Tocolytic agents
- Cervical cerclage
- Pulsed antibiotic therapy
A Team Approach
Preterm birth can be prevented in the majority of circumstances. At the same time, accomplishing such a goal is a team effort. It is extremely important that you, the patient, recognize the part you play on this team. Your self monitoring of uterine contractions in pregnancy is critical to pregnancy health maintenance and should be a part of your obstetrical management. It has been the physician’s experience that this is more effective than electronic monitoring of uterine contractions. The physicians and nurses are also part of the team. Good communication is the key.
Listening is the Important Skill
Perhaps the most important feature in preventing preterm labor and birth is the skill of listening. The pregnant woman must listen to her body as it speaks to her in various ways. Of equal importance, the medical team must listen to the patient as she communicates those signs and symptoms to them. These are the keys to understanding and preventing preterm labor. The prematurity prevention program of the Saint Paul VI Institute has been established with the idea of listening to the patient, interpreting her observations, and implementing successful strategies for the prevention of preterm birth.
Finding Help
If you are at high risk for preterm labor or have previously had a preterm delivery, you can obtain help at the Saint Paul VI Institute. An appointment with the physicians at the Saint Paul VI Institute can be made by calling (402) 390-6600. You may also call for a long-distance telephone consultation with a registered nurse. Indicate that you are at risk for pre-term labor.
PREMENSTRUAL SYNDROME
Premenstrual syndrome (PMS) is a medical condition with a combination of emotional and physical symptoms that can disrupt your health, work, and personal life. The symptoms can occur on a regular basis during the premenstrual phase of the menstrual cycle (7 to 10 days prior to the onset of menstruation). It can be a very debilitating condition.
PMS symptoms are very real. There are 150-200 different symptoms associated with PMS. Common symptoms are bloating, fatigue, irritability, depression, teariness, breast tenderness, carbohydrate craving, weight gain, headache, and insomnia. These begin to occur at least four days prior to menstruation.
It is important to distinguish symptoms which are present premenstrually and those that are present all of the time, e.g. symptoms associated with depression.
Evaluation
Your physician will ask you to begin charting your cycles using CREIGHTON MODEL
FertilityCare™ System. After you have two months of charting, the doctor will recommend a
hormone evaluation which will be timed in cooperation with your charting. By timing the hormone
evaluation based on the information provided by your chart, your physician will be able to determine the
extent to which progesterone and estrogen levels are deficient. Premenstrual syndrome has generally been
considered to be a progesterone deficiency condition. Studies have also shown that decreased levels of
beta-endorphins may be present. In many patients with PMS, a relative degree of hypothyroidism is also
present.
Medical Treatment
In some cases your doctor may prescribe medication to reduce your symptoms. These include:
- Human chorionic gonadotropin (HCG) given in injection form
- Progesterone supplementation
- Naltrexone
If thyroid levels are high or low, a small amount of thyroid medication may be recommended.
A drug used by the Saint Paul VI Institute Physicians in treating PMS is naltrexone. In patients with
low beta-endorphin levels, naltrexone acts to lower the tissue levels of beta-endorphin and allows for
more normal ovarian function. This is especially helpful if anxiety is a major PMS component.
Effectiveness of Treatment
Based on research at the Saint Paul VI Institute for the Study of Human Reproduction, the overwhelming
majority of patients treated according to our protocols feel significant improvement.
ABNORMAL UTERINE BLEEDING
Each month, the endometrium–the lining of the uterus–builds up and sheds. An average menstrual cycle lasts about 28 days, counting from the first day (day 1) of one period through the last day before the beginning of the next. However, a normal cycle may be shorter or longer than this ranging from 21 to 35 days. The menstrual period is the time during the cycle when bleeding occurs and may last from 3 to 7 days.
Abnormal bleeding is bleeding that is not regular, lasts longer, or is heavier than usual. This information describes abnormal uterine bleeding and explains its causes and treatments.
Causes of Abnormal Bleeding
For the first few years after menstrual periods begin, they are often irregular. In older women, menstrual
periods usually become more irregular with the approach of menopause (when the ovaries no longer
function and menstrual periods end), and become lighter or heavier. The irregularity of a woman’s
periods is due to infrequent ovulation ,which is common during these times of life. Menstrual cycles
that persist in being longer than 35 days or shorter than 23 days are not normal and should be checked
by a doctor.
Abnormal bleeding may be the result of a hormonal imbalance. This imbalance can make bleeding longer or shorter than usual, or periods may be more or less frequent.
Besides lack of ovulation and other hormone imbalances, irregular cycles may occur because of weight loss or gain, heavy exercise, stress, illness, or use of drugs. Pregnancy can also cause missed periods or abnormal bleeding. If you think you might be pregnant, you should see your doctor.
Other causes of abnormal of heavy bleeding are:
- Problems with blood clotting
- Infection of the uterus or cervix
- Miscarriage (when a pregnancy is lost before the fetus is able to survive outside the uterus)
- Ectopic pregnancy (pregnancy occurring outside the uterus, most often in one of the fallopian tubes)
- Uterine fibroids (non-cancerous growths that form on the
inside of the uterus, on its outer surface, or within the uterine wall
itself)
- Abnormal growth and thickening of the lining of the uterus
- Polyps (non-cancerous growths) or tumors of the lining of the uterus
- Certain types of cancer, such as cancer of the uterus, cervix, or vagina
- Problems linked to certain birth control methods, such as intrauterine device (IUD) or birth control pills
- Other hormonal problems, such as thyroid disease
Some vaginal bleeding is not from the uterus and may come from other areas.
Diagnosis
To diagnose abnormal uterine bleeding, your doctor will ask you about your medical history and will
give you a physical exam. It is helpful for you to chart the dates and length of your periods by using
the CREIGHTON MODEL FertilityCareTM System. This is an excellent and accurate means of
monitoring the abnormal bleeding. The tests used to diagnose abnormal uterine bleeding may be
based on that charting and the symptoms you are having.
Your doctor may perform a biopsy, in which a small amount of the tissue lining the uterus is removed and looked at under microscope. Cultures of the cervix and vagina may be performed to check for infection.
Tests to determine the cause may include:
- Ultrasound
- Laparoscopy
- Dilation and curettage (D&C)
- Hysterosalpingography
Some of these procedures can be performed in a doctor’s office, while others may be done in a hospital with anesthesia.
Treatment
Treatment for abnormal uterine bleeding will be based on the diagnosis. It may involve surgery or
taking hormones, iron, or other drugs. When hormones are indicated, they are given cooperatively
with the woman’s cycle, based on her NaProTRACKING.
OVARIAN CYSTS
Many women suffer from the recurrence of ovarian cysts. These can become quite painful and when they present themselves, it is common for the physician to recommend either birth control pills for their treatment or surgical intervention sometimes leading to removal of the ovary. In both cases, these treatments are generally unnecessary.
It is helpful to understand the basic workings of the development of the two major types of ovarian cysts:
- Persistent follicular cysts
- Persistent luteal cysts (luteinized unruptured follicle).
With the beginning of the menstrual cycle, the ovary generally does not have any cysts on it or they are very small or left over from the previous cycle. However, as ovulation approaches, there is a cyst that develops on the ovary called the follicle. The egg is located inside the follicle. At the time of ovulation, the follicle ruptures and the egg is released. The follicle then becomes a corpus luteum, which produces progesterone and estrogen. These two hormones prevent the further cystic development on the ovary. When these two hormones are no longer produced (approximately 13 days following ovulation), then menstruation occurs and the process starts all over again.
Persistent Follicular Cysts
With a persistent follicular cyst (which is the least common of the two functional cysts), the growth and development of the follicle is abnormal probably because of outside stress and its hormonal effects. The follicle may grow to a certain size but does not grow any further and stays a follicle. Sometimes this can go on for several weeks. When it does this, it can cause a considerable amount of discomfort and pain and the woman may present to the doctor with pelvic pain (often on one side or the other). Pelvic ultrasound will reveal the presence of a cyst. To know whether or not it is a follicular cyst by ultrasound, one also needs to evaluate the lining of the uterus (the endometrium). If it is in the proliferative phase (the preovulatory phase) by ultrasound examination, then, by definition, this is a follicular cyst.
To prevent these on a long-term basis, the cyclic administration of progesterone in a cooperative fashion with the menstrual cycle can be used.
Persistent Luteal Cysts
With the persistent luteal cyst (or the luteinized unruptured follicle), the follicle grows and develops to a certain point where it would normally rupture and release the egg. However, at that point, it does not rupture and does become luteinized (that is, it causes a corpus luteum to be formed without the follicle rupturing). Progesterone is then produced and eventually the cycle comes to an end. In this case, the unruptured folicle remains on the ovary as a cystic structure and usually increases in size as a woman gets closer and closer to her menstrual flow. This cystic structure can reach 5 to 6 cm in size and become very painful and it is not uncommon then to present her physician with acute abdominal pain. The persistent luteal cyst is far and away the most common of the two functional cysts.
Treatments
Because both of these types of ovarian cysts are related to abnormal hormone function as the primary cause, one can realize that surgical intervention or treatment of these is generally not helpful. In particular, it does not help in the recurrence of these cysts. It may help, of course, in the management of the initial situation but it does not help recurrence of these because surgery does not get to the basic problem that causes these ovarian cysts. Nonetheless, surgical management is often recommended.
The management of these problems is primarily hormonal. Many physicians will recommend the use of birth control pills for this hormonal management, however, that also does not get to the underlying problems.
At the Saint Paul VI Institute, we recommend that the patient learn how to NaProTRACK her menstrual cycles. This allows her to record the various biological markers that key the events of the menstrual cycle. She can do this by learning the CREIGHTON MODEL FertilityCare™ System. With a persistent follicular cyst she will have a prolonged preovulatory phase; with a luteal cyst she may have a prolonged postovulatory phase. In either case, when the patient presents with pelvic pain and an ovarian cyst, an evaluation of the recordings of the biomarkers can be connected with the symptoms that the patient has an ovarian cyst, a reasonably exacting diagnosis can be made.
In both cases, treatment with natural progesterone is the answer! The progesterone can be given cooperatively with the woman’s cycle.
REPEATED MISCARRIAGE
Miscarriage, often called spontaneous abortion by doctors, is the loss of a pregnancy before 20 weeks. It occurs in about 15-20% of all pregnancies. Most happen in the first three months. Three of more miscarriages in a row may be called repeated miscarriage (or habitual abortion). Women who have repeated miscarriages need special tests to try to find the reason for them.
After several miscarriages, you may wonder whether you will ever be able to have a healthy baby. Be hopeful. The chances of having a successful pregnancy are good even after more than one miscarriage. The approach of the doctors at the Pope Paul VI Institute is to diagnose what is wrong, to correct it, and then to support any future pregnancies with hormonal support as soon as the pregnancy is diagnosed.
Causes
Often, the reasons for repeated miscarriage is not known. Sometimes, however, it has a definite
cause. Examples of known causes include:
- Hormone imbalance
- Illnesses in the mother
- Disorders of the immune system
- Abnormalities of the uterus
- Environmental and lifestyle factors
- Chromosomal problems
If you have had more than one miscarriage, each may have had a different cause.
Diagnosis
Because repeated miscarriage has many possible causes, your doctor will need a great deal or
information to diagnose the problem. You will be asked about your medical history and past
pregnancies, as well as your lifestyle. A complete physical exam, including a pelvic exam, is also
important.
The doctors at the Saint Paul VI Institute will ask you to begin charting your cycles using the Creighton Model FertilityCareTM System. By using your chart as a tool, our diagnostic procedures and treatment can be performed and administered more effectively. It allows you and your physician to work in cooperation with your natural cycle. At times cycle abnormalities will become evident in your charting. This information is invaluable to your physician.
Other Diagnostic Procedures
Procedures that might also be done include:
- Laparoscopy and hysteroscopy: This is a surgical procedure in
which a slender, light transmitting instrument, the laparoscope, is used
to view the pelvic organs. The hysteroscope is used to view the inside
of the uterus.
- Blood tests: Blood is drawn and tested for hormone or immune system abnormalities.
- Ultrasound: In this procedure, sound waves are used to view
the internal organs and visualize abnormalities of the pelvic organs.
- Hysterosalpingography: This is an x-ray of the uterus and
fallopian tubes. It is usually taken after the organs are injected with a
small amount of fluid.
- Endometrial biopsy: In this procedure, a sample of the tissue that lines the uterus is taken and looked at under microscope.
Special Care for Future Pregnancies
Sometimes the problem that caused the miscarriages can be treated. Surgery may be effective for
some problems of the uterus and cervix. Treatment with antibiotics can cure infections.
Hormone treatment may be very helpful both before the baby is conceived and during the
pregnancy. The physicians at the Saint Paul VI Institute believe in immediate support with
progesterone and possibly human chorionic gonadotropin depending on the woman’s history.
What You Can Do
If you have had repeated miscarriages, future pregnancies should be planned, diagnosed early and watched carefully. You can improve your chances of having a successful pregnancy in the future by doing the following things:
- Have a complete medical workup before you try to get pregnant
again. It may be that the cause of the miscarriages can be found and
treated by your doctor.
- If you think that you might be pregnant, see your doctor
right away. The sooner you seek prenatal care, the sooner you can
receive any special care that you may need.
- Follow your doctor’s instructions. He or she will tell you
what you need to do to keep yourself and your baby as healthy as
possible.
Coping with Repeated Miscarriage
The loss of a pregnancy–no matter how early or how late–can result in feelings of grief or discouragement that may overwhelm you. For many women, the emotional healing takes longer than the physical healing that follows a miscarriage. Reach out to those closest to you and ask for their comfort and support. Talk to your doctor. Counseling can help both you and your partner if you think that you cannot deal with your feelings alone.
Finally…
Even if you have had repeated miscarriages, you still have a good chance to have a successful pregnancy. Future pregnancies will need prompt, early evaluation. Your doctor will check your pregnancy closely and provide any special care you may need as your baby grows.
DYSMENORRHEA AND PELVIC PAIN
Dysmenorrhea refers to cramps which may occur beginning a few days prior to menstruation and continue for several days during the menstrual flow. These cramps are due to the actual contraction of the muscle of the uterus as it expulses the lining of the uterus at the time of menstruation.
Menstrual cramps can be very severe and immobilizing. They can cause one to miss work, school, etc. It can be associated with nausea, vomiting and rectal pain.
Almost always, this pain is due to some type of underlying organic disease which does lend itself to specific treatment strategies which are very Often successful.
Causes
- Infection
- Endometriosis
- Pelvic adhesions
- Cervical stenosis
Evaluation
Evaluation may include:
- Thorough history and pelvic examination
- Cultures of the cervix and/or uterus
- Pelvic ultrasound
- Diagnostic laparoscopy
- NaProTRACKING of your menstrual cycles
It is helpful in evaluating your pain to NaProTRACK your menstrual cycles. By learning a system for recording the events of your menstrual cycle, you can keep a careful record of your pain.
Treatment
- Oral medications called prostaglandin inhibitors (such as Advil,
Aleve, Motrin, Naprosyn, Anaprox, Cataflam) are often the beginning
treatment
- If these are not helpful, then a diagnostic laparoscopy with laser vaporization of the endometrial implants.
Very often, the birth control pill (BCP) is prescribed for dysmenorrhea. The disadvantage to using the pill to treat this is that it is not diagnosing or correcting the problem. It is masking or suppressing the symptoms. You also have to deal with the annoying and harmful side effects that the BCP causes. More importantly, so many of these changes in the menstrual cycle from the pill have the ability to affect fertility long term. Therefore, in order to have the best chance at preserving fertility and avoiding infertility, it would be best to avoid the birth control pill as a solution to cyclic pain.
ENDOMETRIOSIS

Endometriosis is a condition in which tissue that looks and acts like endometrial tissue is found in places other than the lining of the uterus, such as ovaries, tubes, bowels, outer surface of the uterus and other pelvic structures. Endometriosis may also develop on body tissues located anywhere in the abdomen. These tissues respond to the cycle of changes brought on by the female hormones just as the endometrium normally responds in the uterus. Endometriosis can cause pelvic pain, dysmenorrhea, and infertility.
Diagnosis
An accurate diagnosis can be obtained only by a procedure called laparoscopy. This is an out- patient surgery done under general anesthetic, with a slender light-transmitting telescope that is inserted through a tiny cut made in the lower abdomen. This enables the doctor to view the pelvic organs and to actually see if endometriosis is present.
Treatment
Different types of treatment may be needed for endometriosis:
Laser Laparoscopy
Spots of endometriosis can be removed from their abnormal locations by laser at the time of the diagnostic surgery. This procedure is often recommended for mild and moderate endometriosis. About 50-70% of patients can be treated by laser laparoscopy and can avoid major surgery. Removal by cautery is not recommended as there is an extremely high recurrence rate.
Laparotomy (major surgery)
In cases of severe endometriosis, it may be necessary to have major abdominal surgery. A laser is used in this procedure. With this procedure, you will be in the hospital for a few days and will need 4-6 weeks to recover fully. With surgical treatment, the actual chances of recurrence are low and, when there is recurrence, it is minimal.
Hormone Therapy
Hormone therapy is sometimes recommended as a treatment for endometriosis. The hormones treat the illness by stopping ovulation and have many side effects. They do not correct the problem.
The decision to have surgical treatment…
Many physicians use artificial reproductive technology and do not treat women with infertility by diagnosing and treating their endometriosis. These physicians have not developed the surgical skills necessary to meticulously remove the disease. Dr. Hilgers has been doing this type of surgery for over 30 years and offers expertise in finding and removing spots of endometriosis. He has found endometriosis in 95% of patients who, in a prior laparoscopy by another physician, were told that they did not have endometriosis.
POSTPARTUM DEPRESSION
Postpartum depression is a major depressive disorder which generally begins within the first four weeks following delivery. The symptoms are typically very distressing to the patient and to her family. Changing reproductive hormones and the withdrawal of naturally occurring progesterone following delivery may be a causative factor. Traditional treatment involves psychiatric evaluation and possible antidepressant therapy.
Symptoms
- Depression
- Fatigue
- Changes in appetite
- Changes in sleep
- Thoughts of suicide
- Anxiety
At the Saint Paul VI Institute, the physicians have developed an assessment tool and a treatment protocol for postpartum depression. The patient’s symptoms are evaluated. If indicated, the patient is given a dose of natural progesterone. She makes frequent contact with the physician in an ongoing assessment and additional doses are given as needed.
The effect of the treatment is often quite immediate and the patient reports feeling significantly better. So often, physicians treat this condition with antidepressants. These medications take a significant time to work and also have side effects that many patients find to be hard to tolerate. If you are interested in this service, please call the nurses. Indicate that you are needing help for postpartum depression.
PROGESTERONE SUPPORT IN PREGNANCY

Studies have shown that progesterone support can be helpful in those patients with previous infertility or miscarriage. In additional individuals who can be considered candidates for progesterone evaluation and subsequent supplementation would be those who have had a previous abruptio placentae, previous stillbirth, pregnancy-induced hypertension, previous prematurity, previous premature rupture of the membranes, previous or current intrauterine growth retardation, hyper-irritability of the uterus, congenital uterine anomaly, or patients with cervical cerclage.
Key principles to the use of progesterone in pregnancy are that natural progesterone can be used and that it be started as early as possible in the pregnancy. During the course of the pregnancy, progesterone levels are drawn every two weeks and progesterone is supplemented based on the progesterone level. Through research done at the Saint Paul VI Institute, the physician have developed a graph identifying average level of serum progesterone during the course of the pregnancy. A treatment protocol has been established based on this graph.
Progesterone can be taken by several routes: intramuscularly, vaginally, or orally. Intramuscular dosing provides the best absorption and is generally recommended.
The Institute offers the service of progesterone monitoring to women who are seeing other physicians for all other aspects of their prenatal care. The woman has her blood drawn every two weeks and the serum is sent to the National Reproductive Hormone Laboratory for assay. Dr. Hilgers will then interpret the level and dose the progesterone supplementation accordingly.
If you are interested in this service, please call the nurses and ask for information on getting started (402) 390-6600.
MENOPAUSAL SYMPTOMS AND ESTROGEN REPLACEMENT
During the menopausal period, a woman is often aware of a variety of different symptoms that can be extremely annoying to her.
Symptoms
- Hot flashes
- Irregularity in the menstrual cycle
- Vaginal dryness
- Discomfort with intercourse
- Irritability
- Bloating
- Weight gain
- Carbohydrate craving
- Depression
- Headaches
- Fatigue and insomnia
Treatment
In managing the menopausal symptoms, many physicians recommend estrogen replacement therapy. This causes some perplexing difficulties. For example, if a woman takes estrogen only, the risk of both endometrial and breast cancer goes up. Thus, if a woman takes an estrogen for replacement therapy, she also needs to take progesterone to block or inhibit the effects of the estrogen. In this way, the incidence of endometrial and breast cancer can be normalized.
There are a variety of different approaches to estrogen replacement therapy. There are many different estrogen products available and a number of different progesterone substitutes. The physicians at the Saint Paul VI Institute recommend natural estrogen and progesterone supplements. These medications are bioidentical to what a woman’s own body produces. There are advantages to the use of natural hormones. These are available by prescription through a compounding pharmacist.
The question of how long a woman should be on these hormones is a complicated one and one that needs to be discussed with the woman and her physician.
POLYCYSTIC OVARIAN DISEASE

Polycystic ovarian disease (PCOD) is a condition that is often associated with infertility. The ovaries do not function normally and ovulate only irregularly. The ovaries have multiple cysts that form under the capsule of the ovary. The ovaries are often enlarged. Some 60 percent of women with PCOD will also have endometriosis.
Symptoms
- Amenorrhea
- Long and irregular menstrual cycles
- Obesity
- Hirsuitism (excessive hair growth)
- Hypertension
- Infertility
A complete evaluation includes a thorough hormone profile, a pelvic ultrasound examination, and a laparoscopy.
Treatment
Medical treatment:
Treatment for PCOD is aimed at several factors. A decrease in the production of the male hormones is one aim of treatment. This can be accomplished by giving cortisone-like medication. Fertility treatment can be accomplished by inducing or stimulating ovulation with medications. In order to reduce the incidence of endometrial cancer associated with long and irregular cycles, some type of progesterone withdrawal needs to be implemented on a long-term basis.
Surgical treatment:
An ovarian wedge resection is a surgical procedure in which a wedge of tissue is removed from the ovary and the ovary is subsequently reduced in size and repaired. While this is an older operation, it has been recently resurrected because of significant improvement in our ability to prevent adhesion formation. It is extremely effective in lowering the male hormone production and regulating the menstrual cycles, thus improving fertility. The woman will often go back into regular cycles following this surgery. The pregnancy rate after this procedure is about twice what it is with Clomid.
REVERSE OF TUBAL LIGATION
Women who have had previous tubal ligations can often have their tubal ligation reversed. This is a microsurgical procedure. The area where the ligation occurred is excised and the tubes are microsurgically reconnected. Success of this procedure depends upon the type of tubal ligation that was performed and on the expertise of the microsurgeon. Dr. Hilgers has over thirty years of experience in performing microsurgery. Fortunately, most tubal ligations fall into the category of being able to be reversed. Unfortunately, most insurance companies do not pay for this procedure.
GETTING HELP
If you live in or near Omaha, Nebraska:
For help with one of the above conditions, make an appointment with the director of the Pope Paul VI Institute, Thomas W. Hilgers, MD. Just call the appointments desk at the Pope Paul VI Institute at (402) 390-6600.
An initial appointment interview, which includes a medical history, will be conducted and a personalized and organized evaluation plan will be established. This will lead to an individualized treatment program.
To expedite this program, enroll in a Creighton Model FertilityCare™ System (CrMS) program to learn how to NaProTRACK the menstrual cycle. After two months or two menstrual cycles have been tracked in this fashion, you can see the physician and the process can move quickly. Usually after two cycles of NaProTRACKING™, it only takes two additional months to complete the evaluation.
If you are outside of 150-mile radius of the Omaha metropolitan area:
You can learn the CrMS by attending classes locally or in a location near your hometown. To find or locate a teacher in your area, visit www.fertilitycare.org, or contact Saint Paul VI Institute at (402) 392-0842 or the American Academy of FertilityCare Professionals, 615 S. New Ballas Rd., St. Louis, MO 63141, (314) 569-6495.
Once two cycles or two months of NaProTRACKING™ have been completed, then a good photocopy of that chart can be sent to:
Thomas W. Hilgers, MD, Director c/o Angeli Armstrong
Saint Paul VI Institute
6901 Mercy Road
Omaha, NE 68106-2604
Please include a cover letter, outlining your history and your reason for consultation.
Fees
For a fee of $150, Dr. Hilgers will review the NaProTRACKING™ of your menstrual cycle along with your basic medical history as outlined in your letter. You may also include medical records and previous surgery videos for review. A personal response will be written to you with regard to this evaluation.
Conclusion
If there are any question with regard to your reproductive problems, do not hesitate to write to
Dr. Thomas W. Hilgers at the above address. The staff of Saint Paul VI Institute look forward
to helping you with your women’s health care needs.